Description
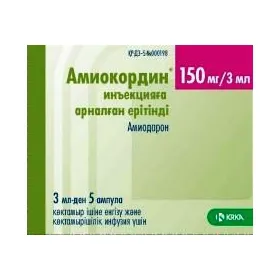
Amiokordin (Amiodarone Hydrochloride) Solution for Injections 150 mg/3 ml. Ampoules 3 ml. N5
Ingredients:
Each 3 ml ampoule contains 150 mg of amiodarone hydrochloride.
Dosage:
The recommended dosage of Amiokordin injection is determined by a healthcare professional based on the patient’s condition. It is usually administered intravenously over a specified period.
Indications:
Amiokordin is indicated for the treatment of life-threatening recurrent ventricular arrhythmias. It is used when other antiarrhythmic agents have failed.
Contraindications:
Do not use Amiokordin if you have hypersensitivity to amiodarone or iodine. It is contraindicated in patients with certain heart conditions and thyroid disorders.
Directions:
Amiokordin should only be administered by healthcare professionals experienced in the management of arrhythmias. The injection should be given slowly to minimize the risk of adverse effects.
Scientific Evidence:
Amiodarone has been extensively studied for its efficacy in treating various arrhythmias. Research published in the American Journal of Cardiology demonstrated the superior antiarrhythmic effects of amiodarone compared to other agents. Clinical trials have shown a significant reduction in ventricular arrhythmias with the use of amiodarone.
Additional Information:
Amiodarone exerts its pharmacological effects by prolonging the action potential and refractory period of cardiac tissues, thus preventing the re-entry of abnormal electrical signals that cause arrhythmias. It also exhibits noncompetitive alpha- and beta-adrenergic blocking properties.
Compared to similar antiarrhythmic drugs, amiodarone is known for its broad spectrum of activity and high efficacy in controlling various types of arrhythmias, especially ventricular arrhythmias. However, it is also associated with a range of potential side effects that require careful monitoring during treatment.