Description
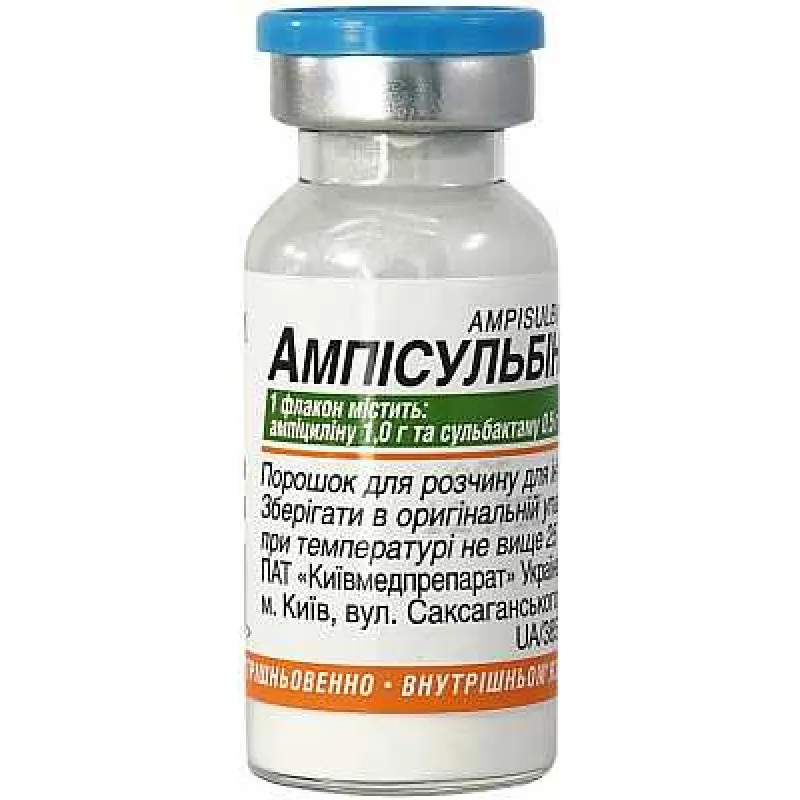
Ampisulbin (Ampicillin, Sulbactam) 1.5 g Vial
Ingredients
Ampicillin and Sulbactam are the active ingredients in Ampisulbin. Ampicillin is a penicillin-type antibiotic, while Sulbactam is a beta-lactamase inhibitor that helps extend the spectrum of Ampicillin.
Mechanism of Action
Pharmacological Properties: Ampicillin inhibits bacterial cell wall synthesis, leading to cell death. Sulbactam enhances Ampicillin’s activity by inhibiting beta-lactamase enzymes produced by resistant bacteria.
Indications
Ampisulbin is indicated for the treatment of various bacterial infections, including respiratory tract infections, skin and soft tissue infections, intra-abdominal infections, and urinary tract infections caused by susceptible bacteria.
Contraindications
Contraindications: Do not use Ampisulbin if you are allergic to penicillins or beta-lactamase inhibitors. It is important to inform your healthcare provider about any allergies or medical conditions before starting treatment.
Side Effects
Clinical trials have shown Ampisulbin to be well-tolerated with a low incidence of side effects.
Usage Instructions
Dosage: The usual dosage of Ampisulbin is 1.5 grams (1 vial) every 6 hours. Dosage may vary based on the severity of the infection and the patient’s condition. It is important to follow the healthcare provider’s instructions.
Directions: Ampisulbin is administered intravenously by a healthcare professional. It is important to complete the full course of treatment as prescribed, even if symptoms improve before the treatment is finished.
Benefits Compared to Analogues
Comparative Effectiveness: Ampisulbin has shown comparable efficacy to other combination antibiotics like amoxicillin-clavulanate in treating various infections. However, its broader spectrum of activity against beta-lactamase-producing bacteria sets it apart.
Suitable Patient Groups
Ampisulbin is suitable for various patient groups including adults, children, and the elderly under appropriate medical supervision.
Storage and Packaging
Ampisulbin should be stored according to the manufacturer’s instructions. The shelf life of the product is as indicated on the packaging.
Clinical Evidence
Studies have shown the efficacy of Ampisulbin in treating a wide range of bacterial infections. Research published in the Journal of Antimicrobial Chemotherapy demonstrated the effectiveness of Ampicillin-Sulbactam combinations in combating multidrug-resistant bacteria.