Description
Anaprilin (Propranolol Hydrochloride) Tablets 0.01 №50
Ingredients:
Each tablet contains propranolol hydrochloride 0.01 mg.
Dosage:
The usual dose ranges from 40 mg to 240 mg per day, depending on the specific condition being treated. Dosage should be tailored to individual patient response.
Indications:
Anaprilin tablets are indicated for the management of hypertension, angina pectoris, cardiac arrhythmias, and prevention of migraine headaches.
Contraindications:
Do not use Anaprilin if you have asthma, bradycardia, or heart block. It is contraindicated in patients with severe heart failure.
Directions:
Take Anaprilin tablets orally with or without food as prescribed by your healthcare provider. Do not discontinue the medication abruptly without consulting your doctor.
Pharmacological Effects:
Propranolol hydrochloride blocks beta-adrenergic receptors, resulting in decreased heart rate, reduced myocardial contractility, lowered blood pressure, and inhibition of renin release from the kidneys, contributing to its antihypertensive effects.
Side Effects:
Common side effects may include fatigue, dizziness, bradycardia, hypotension, and gastrointestinal disturbances. Rare but serious side effects include bronchospasm and heart block.
Benefits Compared to Analogues:
Anaprilin offers comparable efficacy to other beta-blockers in managing cardiovascular conditions while also providing benefits in migraine prevention.
Suitable Patient Groups:
Anaprilin can be used in adults, including the elderly, for the treatment of cardiovascular conditions as indicated by a healthcare professional.
Storage and Shelf Life:
Store Anaprilin tablets in a cool, dry place away from direct sunlight. Check the expiration date on the packaging and do not use the product beyond that date.
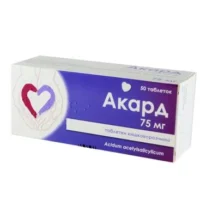
Packaging Description:
Anaprilin tablets are available in a package containing 50 tablets of 0.01 mg propranolol hydrochloride each.
Clinical Evidence and Proven Effectiveness:
Propranolol, the active ingredient in Anaprilin, has demonstrated efficacy in managing hypertension, angina, arrhythmias, and migraine prevention. Clinical trials have shown that propranolol is effective in controlling blood pressure and reducing angina frequency compared to other beta-blockers.