Description
Aritmil (Amiodarone Hydrochloride) Solution for Injections 50 mg. 3 ml. Ampoules N5
Ingredients
Each 3 ml ampoule contains 50 mg of amiodarone hydrochloride.
Mechanism of Action
Amiodarone works by prolonging the action potential duration and refractory period of cardiac tissues, stabilizing the heart’s electrical activity.
Pharmacological Properties
Amiodarone hydrochloride helps in restoring normal heart rhythm and reducing the risk of sudden cardiac death by preventing the reoccurrence of ventricular arrhythmias.
Indications for Use
Aritmil is indicated for the treatment of life-threatening recurrent ventricular arrhythmias, aiming to improve overall survival rates in patients with severe cardiac conditions.
Contraindications
Do not use Aritmil if allergic to amiodarone or any of the solution’s ingredients. It is contraindicated in patients with specific heart conditions and thyroid disorders.
Side Effects
Common side effects of Aritmil include nausea, dizziness, and fatigue. In case of severe side effects or allergic reactions, seek immediate medical attention.
Usage Instructions
The dosage of Aritmil should be individualized based on the patient’s condition and response to treatment. It is typically administered intravenously under medical supervision.
A healthcare professional should administer Aritmil at the prescribed dosage and rate. Regular monitoring of heart function and thyroid levels is essential during treatment.
Benefits Compared to Analogues
Aritmil has shown high efficacy in managing ventricular arrhythmias, as demonstrated in studies. Its ability to reduce the incidence of ventricular arrhythmias and improve survival rates sets it apart from other treatments.
Suitable Patient Groups
Aritmil is suitable for adult patients with life-threatening recurrent ventricular arrhythmias. Special caution and individualized dosing are required for elderly patients and those with compromised liver or kidney function.
Storage Conditions and Shelf Life
Store Aritmil as per the instructions provided on the packaging. Ensure proper storage conditions to maintain the integrity and efficacy of the product. Check the expiration date before use.
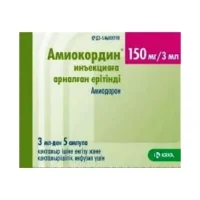
Packaging Description
Aritmil is available in ampoules containing 50 mg of amiodarone hydrochloride in a 3 ml solution. Each package contains 5 ampoules for injections.
Scientific Evidence
Amiodarone, the active ingredient in Aritmil, has been extensively studied for its efficacy in managing ventricular arrhythmias. Research published in the American Journal of Cardiology has shown that amiodarone is highly effective in reducing the incidence of ventricular arrhythmias and improving overall survival rates in patients with severe cardiac conditions.