Description
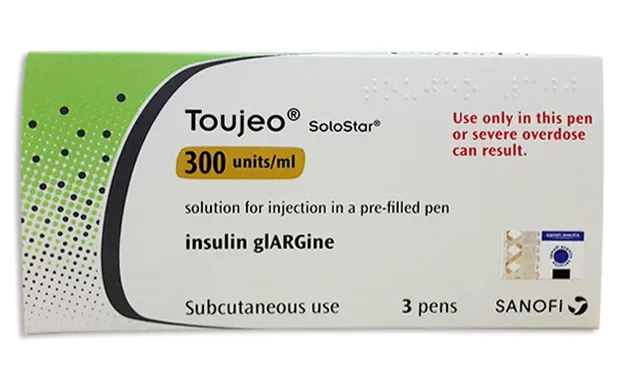
Tojeo SoloStar (Insulin Glargine) Solution for Injections 300 IU/ml – 1.5 ml – Carton with Syringe
Ingredients:
- Tojeo SoloStar contains insulin glargine as the active ingredient.
- Other ingredients include glycerol, metacresol, zinc oxide, and water for injections.
Dosage:
The recommended dosage of Tojeo SoloStar is determined by the healthcare provider based on individual needs. It is administered subcutaneously once daily at the same time each day.
Indications:
Tojeo SoloStar is indicated for the treatment of diabetes mellitus in adults, adolescents, and children aged 6 years and above.
Contraindications:
Tojeo SoloStar is contraindicated in patients with hypersensitivity to insulin glargine or any of the excipients in the formulation.
Directions:
Tojeo SoloStar should be administered subcutaneously into the thigh, upper arm, or abdomen. Injection sites should be rotated to reduce the risk of lipodystrophy.
Scientific Evidence:
Studies have shown that insulin glargine provides long-acting basal insulin coverage with a consistent effect on blood glucose levels. Clinical trials have demonstrated its efficacy in improving glycemic control in patients with diabetes.
Additional Information:
It is important to monitor blood glucose levels regularly when using Tojeo SoloStar to adjust the dosage as needed.
Insulin glargine works by mimicking the action of naturally produced insulin in the body. It helps regulate glucose metabolism by promoting the uptake of glucose into cells for energy production, leading to a reduction in blood sugar levels and prevention of diabetes complications.
Clinical studies have compared the effectiveness of insulin glargine products like Tojeo SoloStar with other long-acting insulins. Research has shown that insulin glargine demonstrated similar efficacy but with a lower risk of hypoglycemia compared to other basal insulins.